Abstract
This essay will focus on how the British understood and responded to the cholera epidemics that swept Britain four times from the early eighteen-thirties to the mid-eighteen-sixties, with special attention to the first epidemic and how it related to political Reform.
Cholera first arrived at a time of significant political change that affected the way it was understood by various groups within Britain. The poor, the ill-defined middle-classes (comprising diverse groups of people from small business owners and clerks to owners of large factories and many professionals like lawyers and doctors), and the traditional land-owning elite were all in the process of redefining their access to political power through the gradual extension of the right to vote. The cholera epidemics, poorly understood by medical experts of the time, were understood by these groups in different ways as government and the medical profession experimented with responses. Cholera provides a useful lens to see how an externally generated stressor like an epidemic intersects with other cultural and historical forces, giving insight not only into medical but also political and cultural history.
Between 1832 and 1866, four cholera epidemics struck Great Britain, as part of pandemic outbreaks that affected the entire globe. In 1817, before the first British epidemic, there had been a smaller epidemic that spread in Europe but did not cross the channel. The 1832 epidemic was the first one to enter Britain—and also spread to the Americas and ![]() Australia—and wreaked panic as well as high death rates where it struck. The 1848 second epidemic was global and caused high death rates in Britain. By the mid-1850s, Britain was more ready when cholera again entered the islands but still suffered considerable mortality. The last and least, but still murderous, British epidemic was in 1866. After that, in the 1870s and 90s, cholera did sweep across the European continent again but did not cross the channel in epidemic force.
Australia—and wreaked panic as well as high death rates where it struck. The 1848 second epidemic was global and caused high death rates in Britain. By the mid-1850s, Britain was more ready when cholera again entered the islands but still suffered considerable mortality. The last and least, but still murderous, British epidemic was in 1866. After that, in the 1870s and 90s, cholera did sweep across the European continent again but did not cross the channel in epidemic force.
In the 1830s, the disease was still unfamiliar in most of the world beyond parts of the Indian subcontinent. Terrified patients had never seen such symptoms before, and doctors were helpless to do anything but try remedies that they thought had worked for other diseases. These remedies, from the relatively merciful giving of opiates to more aggressive approaches such as bleeding or burning the skin, were largely worthless, as were most theories of how the disease was transmitted (including, but not limited to, bad weather, foul smells, electro-magnetism and divine vengeance). We now believe cholera to be a waterborne disease caused by a comma-shaped bacillus called vibrio cholerae, which is transmitted between humans via the fecal-oral route. It usually enters the body through contaminated water or food and then multiplies in the intestines. Although easily treatable today in developed areas with abundant clean water and medical care, cholera remains an important epidemic disease in parts of Africa, ![]() India, and Latin America and it has recently taken thousands of lives in
India, and Latin America and it has recently taken thousands of lives in ![]() Haiti. Untreated, it can kill within a few days through rapid dehydration, caused by copious, uncontrollable diarrhoea. As the disease progressed, the diarrhoea becomes a clear, straw colored fluid, described in the period as resembling “rice water.” It is hard to see and can quickly soak bedding and floor coverings. As people in the 1830s did not understand what caused the disease nor, indeed, know about germs (which were not understood until much later in the late-nineteenth century), caregivers did not even know to wash their hands after tending the sick. In an era without running water in most homes, and with many people living in small spaces, it was easy for contamination to spread. And in industrial early nineteenth-century cities with rapidly growing populations and no sewer systems, most people disposed of their waste in cesspits or in the streets. From there, it eventually ended up in rivers that provided drinking water, spreading it far beyond its origin. Because dehydration was so rapid, apparently healthy people became weak very quickly. Their appearance was frightening: skin shrivelled, eye sockets collapsed, and complexion blue from oxygen deficiency. Patients first screamed and thrashed as their muscles spasmed, then lay exhausted and unresponsive, and soon died—sometimes within the first 24 hours. Mortality for cases who reached the stage of weakness and “collapse” was around fifty percent. [See Fig. 1.]
Haiti. Untreated, it can kill within a few days through rapid dehydration, caused by copious, uncontrollable diarrhoea. As the disease progressed, the diarrhoea becomes a clear, straw colored fluid, described in the period as resembling “rice water.” It is hard to see and can quickly soak bedding and floor coverings. As people in the 1830s did not understand what caused the disease nor, indeed, know about germs (which were not understood until much later in the late-nineteenth century), caregivers did not even know to wash their hands after tending the sick. In an era without running water in most homes, and with many people living in small spaces, it was easy for contamination to spread. And in industrial early nineteenth-century cities with rapidly growing populations and no sewer systems, most people disposed of their waste in cesspits or in the streets. From there, it eventually ended up in rivers that provided drinking water, spreading it far beyond its origin. Because dehydration was so rapid, apparently healthy people became weak very quickly. Their appearance was frightening: skin shrivelled, eye sockets collapsed, and complexion blue from oxygen deficiency. Patients first screamed and thrashed as their muscles spasmed, then lay exhausted and unresponsive, and soon died—sometimes within the first 24 hours. Mortality for cases who reached the stage of weakness and “collapse” was around fifty percent. [See Fig. 1.]
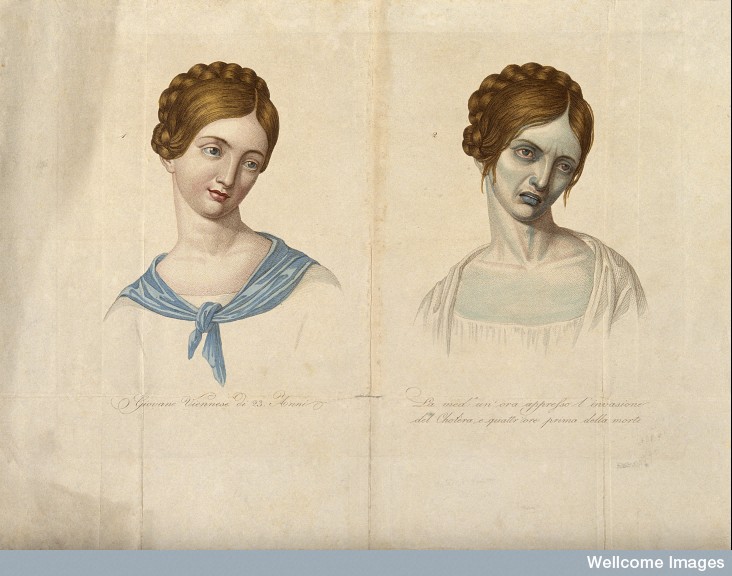
Figure 1: A young Venetian woman, aged 23, depicted before and after contracting cholera. Coloured stipple engraving. Courtesy of Wellcome Library
A rigorous quarantine might well have saved the island nation from the dramatic mortality seen on the continent, and quarantine was initially tried in late 1831, to be imposed upon ships coming from the ![]() Baltic. But merchants were outraged at quarantine’s threats to trade, and many did not believe quarantine would work anyway, and so it was not well enforced. After all, quarantine had apparently already failed in the case of Eastern Europe’s (much more porous) borders, business interests argued. Besides, many people thought that probably the cholera was a figment of the imagination anyway or, at least, an exaggerated threat. Despite the sporadically enforced quarantine, cholera entered Britain in the port town of
Baltic. But merchants were outraged at quarantine’s threats to trade, and many did not believe quarantine would work anyway, and so it was not well enforced. After all, quarantine had apparently already failed in the case of Eastern Europe’s (much more porous) borders, business interests argued. Besides, many people thought that probably the cholera was a figment of the imagination anyway or, at least, an exaggerated threat. Despite the sporadically enforced quarantine, cholera entered Britain in the port town of ![]() Sunderland in fall of 1831. Early victims were not positively identified as dying from cholera—local doctors had never seen it, only heard about it from Continental sources, so they were likely to declare the deaths of the earliest cholera sufferers as resulting from other causes—but the first “official” case was identified in late October. William Sproat, a 60 year old shipyard worker, succumbed within three days after calling in the doctor, followed by his family, who had nursed him. From there, it quickly spread, as has been extensively documented (see especially Durey and Morris for Britain; for
Sunderland in fall of 1831. Early victims were not positively identified as dying from cholera—local doctors had never seen it, only heard about it from Continental sources, so they were likely to declare the deaths of the earliest cholera sufferers as resulting from other causes—but the first “official” case was identified in late October. William Sproat, a 60 year old shipyard worker, succumbed within three days after calling in the doctor, followed by his family, who had nursed him. From there, it quickly spread, as has been extensively documented (see especially Durey and Morris for Britain; for ![]() France, Kudlick, and Delaporte; and for
France, Kudlick, and Delaporte; and for ![]() Germany, R. Evans). It left behind 215 documented deaths in Sunderland alone, and probably many more listed under other causes or not recorded, and swept away many thousands more throughout the Kingdom before it ebbed in late summer.
Germany, R. Evans). It left behind 215 documented deaths in Sunderland alone, and probably many more listed under other causes or not recorded, and swept away many thousands more throughout the Kingdom before it ebbed in late summer.
When cholera was first discussed by the British public, as it marched across the continent in 1831 and 32, Britons were already preoccupied with a big political topic: Parliamentary and voting Reform. Reform had been a perennial focus over the last several years, but in the form that finally became law it had been hotly debated from June 1830, when dissolute King George IV died. After long discussion, it was passed in Commons and then defeated in the House of Lords in 1831. Rioting ensued, and a revised Bill was brought forward subsequently that year. Through the spring of 1832, the Lords dithered and the mood of the country grew increasingly tense. When it finally passed, on 7 June 1832, it gave more representation to large cities that had gained population as a result of the Industrial Revolution and eliminated representation for areas where the population had diminished to the point that a Member of Parliament was often elected by only a handful of landowners. Most importantly, although it didn’t increase the size of the electorate that much—it is estimated to have raised it from about 400,000 to 650,000, allowing one out of six adult males to vote—it began to redistribute some power from landowners to the mercantile and manufacturing class, as it allowed those who did not own, but merely rented valuable property (as was common in towns, for example), to vote. The full title of the Reform Bill was An Act to amend the representation of the people in England and ![]() Wales. (Separate reform bills were passed in the same year for
Wales. (Separate reform bills were passed in the same year for ![]() Scotland and
Scotland and ![]() Ireland).
Ireland).
As authorities argued over cholera’s causes, treatment, and prevention, various publics formed their own opinions of what was going on. Middle-class and working people who hoped that Reform would bring them representation in Parliament suspected that the talk of cholera was being used to distract the populace from Reform in the interests of the elite retaining control of political power. Many people were not sure the cholera was even real; perhaps it was a bugbear invented to let the powerful take control of the poor’s few belongings, or even their bodies. After all, scandal was rife about medical schools paying grave robbers for bodies to use for dissection. In Scotland, William Burke and William Hare had been convicted in ![]() Edinburgh in 1829, not only of grave robbing to sell to anatomists, but of providing themselves with merchandise through several actual murders in 1827 and 1828. Outrage against graverobbing spurred Parliament to deliberate on a “Dead Body Bill” or Anatomy Act, passed in 1832 (See Richardson). The Act, which provided that bodies of paupers not claimed within 48 hours by family members able to pay for interment would be available for dissection, was designed to prevent grave robbing by providing a steady source of bodies, but it also had the effect of making the poor particularly vulnerable to the seizure of their bodies after death. People diagnosed with cholera were often forcibly removed in the name of public safety to specially designated “cholera hospitals,” where, of course, many died, outraging the feelings of families and fueling suspicions that they were actually being killed. In response, many families hid their sick from inspectors or resisted their removal. In the minutes of a meeting of the
Edinburgh in 1829, not only of grave robbing to sell to anatomists, but of providing themselves with merchandise through several actual murders in 1827 and 1828. Outrage against graverobbing spurred Parliament to deliberate on a “Dead Body Bill” or Anatomy Act, passed in 1832 (See Richardson). The Act, which provided that bodies of paupers not claimed within 48 hours by family members able to pay for interment would be available for dissection, was designed to prevent grave robbing by providing a steady source of bodies, but it also had the effect of making the poor particularly vulnerable to the seizure of their bodies after death. People diagnosed with cholera were often forcibly removed in the name of public safety to specially designated “cholera hospitals,” where, of course, many died, outraging the feelings of families and fueling suspicions that they were actually being killed. In response, many families hid their sick from inspectors or resisted their removal. In the minutes of a meeting of the ![]() St. Olave’s District Board of Works, it is recorded that, “The bodies of those who have died have been removed as speedily as possible, but in the case of the young woman who died in
St. Olave’s District Board of Works, it is recorded that, “The bodies of those who have died have been removed as speedily as possible, but in the case of the young woman who died in ![]() Vine Street, about 200 and [sic] 300 persons collected to prevent the removal of the body. It was, therefore, not persisted in” (“St. Olave’s District Board of Works” 4). Although violence against doctors and government officials was not as prevalent as it was on the continent, there was still some rioting and vandalism of cholera hospitals. Meanwhile, property owners compelled to spend money to clean up “nuisances” or merchants whose businesses were hurt by cholera panic were also suspicious of the motives of government.
Vine Street, about 200 and [sic] 300 persons collected to prevent the removal of the body. It was, therefore, not persisted in” (“St. Olave’s District Board of Works” 4). Although violence against doctors and government officials was not as prevalent as it was on the continent, there was still some rioting and vandalism of cholera hospitals. Meanwhile, property owners compelled to spend money to clean up “nuisances” or merchants whose businesses were hurt by cholera panic were also suspicious of the motives of government.
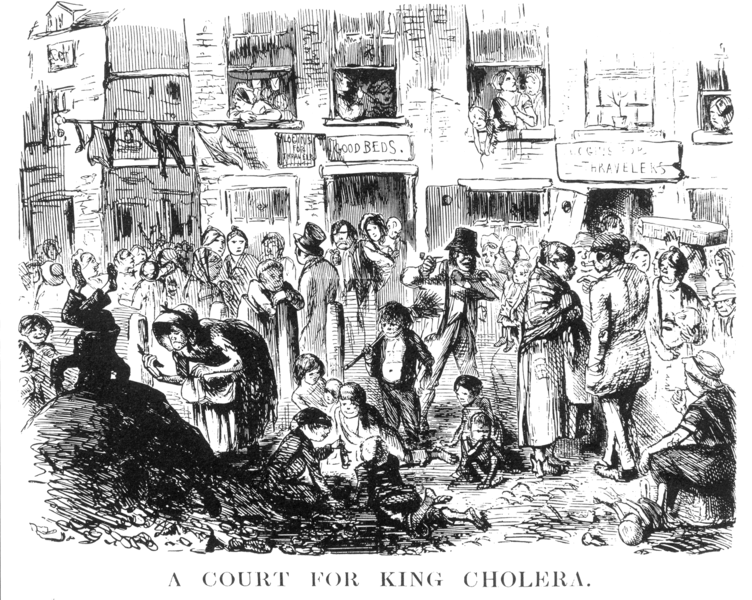
So the first epidemic was immediately understood in a context of class struggle. The clergy was the traditional source of local authority at times like these, but the Church of England was also under considerable stress from a religious reform movement, which had in the late 1820s sought to grant other Protestant denominations and even Catholics more political representation (historically, Catholics, for example, could not be Members of Parliament, whereas Bishops of the Church of England sat ex officio in the House of Lords). These religious disputes had a class component: although not always true, in general, Church of England members tended to be wealthier, upper class, and from Southern England, where power was historically seated. Lower middle-class industrial and manufacturing districts to the North and West tended to include more dissenters, and Catholicism was associated with the Irish, both those in Ireland and the many poor Irish in England. So, the same class hostility that was linked to political Reform was closely connected to religious conflict, and this undermined the authority of the established Church to speak for the larger community in this crisis. When the Church of England, backed by Parliament, declared a day of fasting and prayer to ward off the cholera, which they attributed to divine punishment, labor organizations satirically declared a feast day for their readers, arguing that the poor had already fasted enough. Meanwhile, political Reformers observed, sometimes mockingly and sometimes in earnest, that if God was angry, it was probably because Reform was being stalled. Radical press and labor organizations emphasized the absurdity of the solutions proposed by the upper classes for an audience in very different circumstances. Henry Hetherington of The Poor Man’s Guardian—who himself died of cholera in 1849 (Durey 195)—ridiculed the notion of the general fast-day through several issues, beginning on 11 Feb. 1832: “a general fast is all very fair; for God knows that as yet the fasting has been partial enough . . . . if not merely fasting but if the most abject want be any propitiation for the evil, never would CHOLERA MORBUS have made its appearance among us!” (Hetherington 1).
Such gestures dramatized the opposing physical circumstances in which rich and poor lived. Ballads that were printed on single sheets, and given away or sold for pennies on the street, promoted the views of Reformers: one example warns: “They tell such tales our hearts to fear/ Of Cholera raging here and there,/ But bread, pudding, and good cheer,/Will drive the Cholera Morbus . . . //But Reformers will not be deceived,/ For by them it is all agreed/ That one and all we shall be freed,/ In spite of the Cholera Morbus” (“A New Song”). Meanwhile, by both the poor and merchants, the doctors and clergy might be seen as allies of the elite. In one small town, for example, notices saying “No cholera at Ely/ The Parsons Liars/And Doctors Pickpockets” were pasted over cholera warning handbills distributed by the Board of Health (Holmes 32-33). Thus, the middle-classes were often agnostic or actively skeptical on the issue of cholera’s threat and were inclined to be more concerned with gaining political representation and avoiding disruptions to trade.
Although most popular responses to the cholera were political and religious, public policy focused on two initial responses: quarantine to keep the cholera out of Britain and, subsequently, cleaning up “nuisances”: that is, things that were perceived as smelly and dirty. Since disease was largely believed to be caused by atmospheric problems, and by bad smells, cleaning up open cesspits, garbage piles and so forth was thought to be a way to avoid the spread of disease. This was viewed as more of an engineering problem (how do you get rid of this stuff?) and a legal problem (how do you make property owners clean up their property?) than a medical problem, per se. After all, one didn’t need a trained professional to tell if something smelled bad.
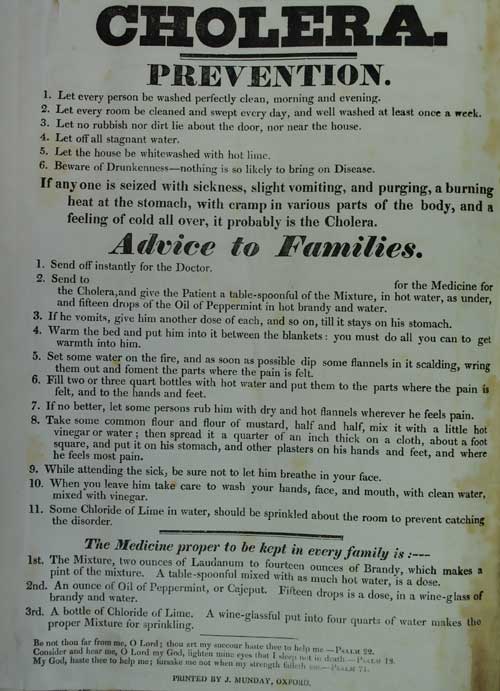
Figure 2: “Cholera Prevention Notice. Notices like this were widely posted. Note the emphasis on temperance. By kind permission of the Oxfordshire Health Archives.
So at first, it seemed logical to focus on cleanliness, which was considered an engineering and moral problem, rather than bringing in medical expertise. Chadwick did work with some like-minded people who did happen to be doctors, however, especially Thomas Southwood Smith, to produce a detailed report on The Sanitary Condition of the Labouring Population (1842), with a supplementary report published in 1843. Although the events of 1832 and Chadwick’s reports showed plenty of cause for sanitary legislation, it wasn’t until rumours of cholera’s return that a Public Health Act was finally passed in 1848. Chadwick was made a commissioner for London’s Metropolitan Commissioner of Sewers from 1848 to 1849, which had a good deal to do with sanitary inspection, and of the General Board of Health from its inception in 1848 to its abolition in 1854, when it was replaced by local boards. Chadwick angered many people, as he was considered abrasive and high-handed. One the other hand, he managed against all odds—including traditional fatalism about epidemics fed by beliefs about divine punishment, bureaucratic inertia, and local resistance by both individuals and organizations of ratepayers (taxpayers) who resented the cost of sanitary remediation—to get a serious sanitary movement started.
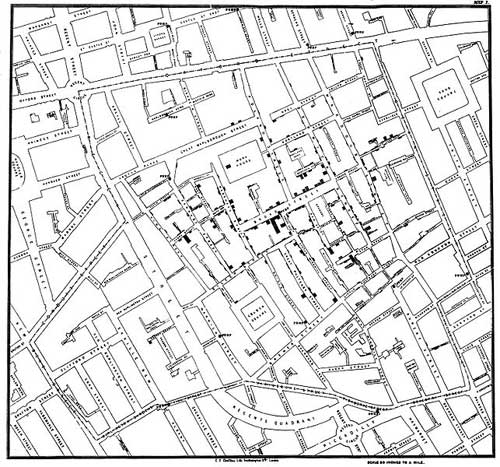
Figure 4: Snow’s Map of Cholera in St James’s Parish (1854), showing the locations of individual deaths in relation to the location of the water pump
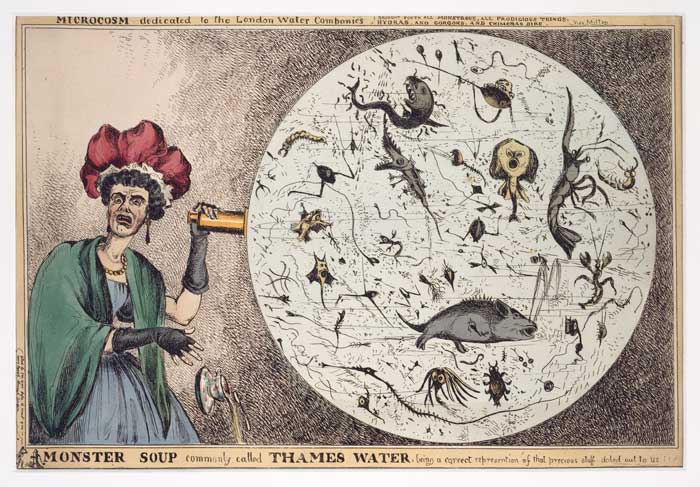
Figure 5: “Cartoon of a woman horrified by a microscopic view of drinking water from the Thames.” Courtesy of the World Digital Library
Medicine was, at the time, rapidly developing as a profession. New scientific breakthroughs were changing the practice of medicine dramatically, and the profession was beginning to police itself, insisting on more formal training and certification than ever before. What would come to be understood over the course of the period as “public health”—especially in relationship to epidemic disease and sanitary issues—was just beginning to emerge in the 1840s but would play an increasingly central role in the state’s relationship to Britons. This centrality was in part made possible by the increase in epidemic diseases related to industrial urbanization, but cholera, as a dramatic newcomer to the scene, gave medics a significant opportunity to take center stage. Because of the effects of the 1848 Public Health Act, and the subsequent development of central coordination of mortality information, we have much more information about what followed than we do about 1832. The epidemic of 1848-9 exacted a much more devastating toll than the first. It is hard to get accurate numbers, but the official reports of the period taken from statistician and medical man William Farr’s Report on the Mortality of Cholera in England in 1848–49 confirm that the English government then believed that 55,181 deaths had occurred from cholera in England alone, besides 28,900 from “diarrhoea” (qtd. in Tanner 588).
By 1848, continental Europe was experiencing a great deal of political unrest and revolutionary activity. Britain had also suffered an economically difficult decade, and the working classes who had not seen increased representation under the 1832 Bill were agitating in the late 1840s for a “People’s Charter” that would guarantee them more direct political representation. Although the Charter was defeated, and there was not in fact the political fallout that many feared, it seemed to many that cholera was a disease that always accompanied—or was accompanied by—class conflict and the threat of revolution. The now enfranchised middle classes, who had been likely to oppose the intervention of government in 1832, were in the late 1840s more apt to see the government as protecting them from an epidemic caused by dirty poor people—especially the destitute Irish who had flooded into England, fleeing starvation in their own country caused by the potato famine that began in 1844 and continued for several years. Still, however, when that intervention meant that middle-class property owners were asked to incur expense cleaning up “nuisances” such as dung heaps or garbage from slaughter houses on their property, or help with sanitary problems by paying higher local taxes, they often resisted.
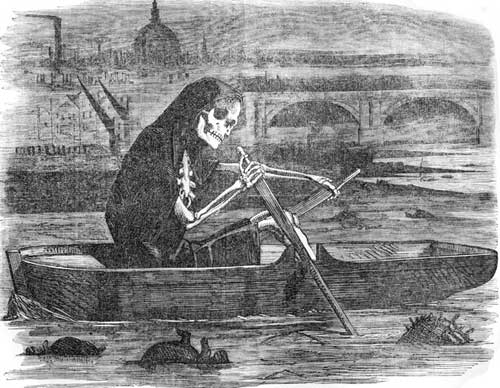
Figure 6. “The Silent Highwayman: Your Money or your Life," from cartoon in Punch Magazine 35 (1858): 137
After the earlier disasters, the 1866 epidemic was relatively small and historically unimportant by comparison. The mechanism of contagion was more clearly understood and modern sewerage was functioning in the large cities. Although voting reform in the guise of The Representation of the People Act (Second Reform Act), which passed in 1867, was being discussed as cholera arrived in 1866, and although that Act was numerically much more significant, doubling the electorate and allowing many working men to vote, it was less politically explosive. In part this was because the 1860s were fairly prosperous, reducing the discontent of the unenfranchised. But it was also because the principle of allowing a vote to men with some basic financial stability had been recognized in 1832, so later reforms were perceived as incremental rather than revolutionary. Still, it would take a few more reforms until 1918 to extend the national vote to all adult male householders in England and Wales (the extension of the vote even to a minority of women in 1918 was much more difficult). Universal suffrage for adults in national and local elections was not established finally until 1948.
Although some historians have reacted against what they see as cholera’s undue prominence in many historical accounts of the period, cholera had a very important cultural impact that was disproportionate to its actual mortality. Cholera killed far fewer than other nineteenth-century epidemics like typhoid or typhus, but those were diseases with which Britons were familiar, and, so, their depredations seemed less dramatic and received less publicity. Of course, cholera did not by itself cause the sanitary movement. But the combination of the development of statistical techniques that allowed people to conceive of and track disease as a large scale event, Reform agitation around the first epidemic, and changing understandings of the role of the state combined with the dramatic eruption of a new disease to provide unique historical opportunities. Later, doctors and other professionals and legislators would be able to shape the movement begun under Chadwick into the foundations for modern public health legislation, such as a belief in the right to live in a clean environment.
Thus, the conflict over the meaning of the disease that characterized the early discussions of clergy and Reformers was largely over by 1866. Other kinds of political issues took center stage in this relatively prosperous period, such as the relation of Britain to its empire and foreign policy issues. But the connections between health and government highlighted by the original combination of the first epidemic with the first great Reform Bill of 1832 continued to resonate, as public health became and remained a major component of government responsibility. These concerns continued to shape discussions of the role of government and its relation to individual rights up to the present day.
HOW TO CITE THIS BRANCH ENTRY (MLA format)
published May 2012
Gilbert, Pamela K. “On Cholera in Nineteenth-Century England.” BRANCH: Britain, Representation and Nineteenth-Century History. Ed. Dino Franco Felluga. Extension of Romanticism and Victorianism on the Net. Web. [Here, add your last date of access to BRANCH].
“A New Song on the Cholera Morbus.” Quarto Broadsheet. Wheeler, 1831 [?]. London Guildhall, Ephemera Collection. Print.
Chadwick, Edwin and Thomas Southwood Smith. Report on the Sanitary Condition of the Labouring Population. London: Clowes, 1842. Print.
—. Report on the Sanitary Condition of the Labouring Population of Great Britain. A Supplementary Report on the Results of a Special Inquiry into the Practice of Internment in Towns. London: Clowes, 1843. Print.
Delaporte, François. Disease and Civilization: The Cholera in Paris, 1832. Trans. Arthur Goldhammer. Foreword by Paul Rabinow. Cambridge: MIT P, 1986. Print.
Durey, Michael. The Return of the Plague: British Society and the Cholera, 1831-2. Dublin: Gill and Macmillan Humanities P, 1979. Print.
Evans, Richard J. Death in Hamburg: Society and Politics in the Cholera Years, 1830‑1910. Oxford: Clarendon P, 1987. Print.
Farr, William. Report on the Mortality of Cholera in England in 1848-49. London: W. Clowes and Sons for Her Majesty’s Stationery Office, 1852. Print.
Gilbert, Pamela K. Cholera and Nation. Doctoring the Social Body in Victorian England. Albany: SUNY P, 2008. Print.
–. The Citizen’s Body: Desire, Health, and the Social in Victorian England. Columbus: The Ohio State UP, 2007. Print.
Hamlin, Christopher. Public Health and Social Justice in the Age of Chadwick: Britain, 1800-1854. Cambridge: Cambridge UP, 1998. Print.
Hetherington, Henry. The Poor Man’s Guardian 1 (1832): 1. Print.
Holmes, Reginald. That Alarming Malady. Ely: Ely Local History Publication Board, 1974. Ely Local History Series. Print.
Kudlick, Catherine. Cholera in Post‑Revolutionary Paris: A Cultural History. Berkeley: U of California P, 1996. Print.
Morris, R.J. Cholera 1832: The Social Response to an Epidemic. London: Croom Helm, 1976. Print.
Richardson, Ruth. Death, Dissection and the Destitute. London: Routledge, 1987. Print.
Snow, John. On the Mode of Communication of Cholera. 2nd ed., much enlarged. London: John Churchill, 1855. Print.
—. “On the Pathology and Mode of Communication of Cholera.” London Medical Gazette 44 (2 November 1849): 745-52; (30 November 1849): 923-29. Print.
“St. Olave’s District Board of Works.” Minutes of meeting. The South London Press 25 August 1866: 4. Print.
Tanner, Thomas Hawkes. The Practice of Medicine, 6th Ed. Philadelphia: Lindsay and Blakiston, 1874. Google Books. Web. 14 May 2012.